Vitamin B12 deficiency
B12 deficiency presents with macrocytic, megaloblastic anaemia ranging
from mild to severe (Hb <6.0g/dL).
Symptoms
are those of chronicanaemia, i.e. fatigue, dyspnoea on effort, etc. Neurological symptoms may
also be present —classically peripheral paraesthesiae and disturbances of
position and vibration sense. Occasionally neurological symptoms occur
with no/minimal haematological upset. If uncorrected, the patient may
develop subacute combined degeneration of the spinal cord7permanently
ataxic.
Pathophysiology
B12 is required for DNA synthesis; B12 is alsorequired for neurological functioning. B12 is absorbed in terminal ileum
after binding to intrinsic factor produced by gastric parietal cells. Body
stores of B12 are 2–3mg (sufficient for 3 years). B12 is found in meats, fish,
eggs and dairy produce. Strictly vegetarian (vegan) diets are low in B12
although not all vegans develop clinical evidence of deficiency.
Presenting haematological abnormalities
1 Macrocytic anaemia (MCV usually >110fL). In extreme cases RBC
anisopoikilocytosis can result in MCV values lying just within normal
range.
2 RBC changes include oval macrocytosis, poikilocytosis, basophilic stippling,
Howell–Jolly bodies, circulating megaloblasts.
3 Hypersegmented neutrophils.
4 Leucopenia and thrombocytopenia common.
5 Bone marrow shows megaloblastic change; marked erythroid hyperplasia
with predominance of early erythroid precursors, open atypical
nuclear chromatin patterns, mitotic figures and ‘giant’ metamyelocytes.
2 Iron stores usually
2 Serum B12 5.
2 Serum/red cell folate usually 6 or 4.
2 LDH levels markedly 4 reflecting ineffective erythropoiesis.
2 Autoantibody screen in pernicious anaemia: 80–90% show circulating
gastric parietal cell antibodies, 55% have circulating intrinsic factor antibodies.
chemical formula of vitamins b12
Note:
parietal cell antibodies are not diagnostic since found innormals; IFA is only found in 50% of patients with PA but is diagnostic.
Causes of B12 deficiency
Pernicious anaemia Commonest, due to autoimmune gastric
atrophy resulting in loss of intrinsic
factor production required for absorption
of B12. Incidence increases >40
years and often associated with other
autoimmune problems, e.g. hypothyroidism.
Following total gastrectomy May develop after major partial gastrectomy.
Ileal disease Resection of ileum, Crohn’s disease.
Blind loop syndromes E.g. diverticulae or localised inflammatory
bowel changes allowing bacterial
overgrowth which then competes for
available B12.
Fish tapeworm Diphyllobothrium latum.
Malabsorptive disorders Tropical sprue, coeliac disease.
Dietary deficiency E.g. vegans.
Management of B12 deficiency
1. Identify and correct cause if possible.
2. Above investigations are undertaken and a test of B12 absorption is
carried out (e.g. Schilling test). Urinary excretion of a test dose of B12
labelled with trace amounts of radioactive cobalt is compared with
excretion of B12 bound to intrinsic factor*; the test is done in two
parts. B12 malabsorption corrected by intrinsic factor is diagnostic of
pernicious anaemia (in absence of previous gastric surgery).
3. Management —hydroxocobalamin 1mg IM and folic acid PO should be
given immediately.
4. Supportive measures —bed rest, O2 and diuretics may be needed
while awaiting response. Transfusion is best avoided but 2 units of concentrated
RBCs may be used for patients severely compromised by
anaemia (risk of precipitating cardiac failure); hypokalaemia is occasionally
observed during the immediate response to B12 and serum [K+]
should be monitored.
5. Response apparent in 3–5d with reticulocyte response of >10%;
normoblastic conversion of marrow erythropoiesis in 12–24h. Patients
frequently describe a subjective improvement within 24h.
6. B12 replacement therapy —initially hydroxocobalamin 5 ¥ 1mg IM
should be given during the first 2 weeks, thereafter maintenance injections
are needed 3-monthly.
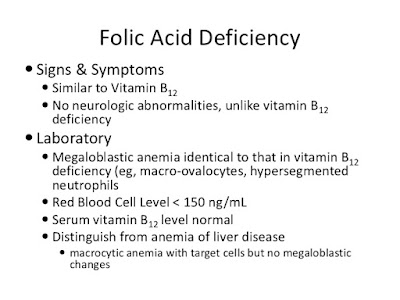
Folate deficiency (Vitamin B9)
Folate deficiency represents the other main deficiency cause of megaloblastic
 anaemia; haematological features indistinguishable from those of
anaemia; haematological features indistinguishable from those ofB12 deficiency. Distinction is on basis of demonstration of reduced red cell
and serum folate.
Megaloblastic anaemia patients should never receive empirical treatment
with folic acid alone. If they lack B12, folic acid is potentially
capable of precipitating subacute combined degeneration of the
cord.
Pathophysiology
Adult body folate stores comprise 10–15mg; normal daily requirementsare 0.1–0.2mg, i.e. sufficient for 3–4 months in absence of exogenous
folate intake. Folate absorption from dietary sources is rapid; proximal
jejunum is main site of absorption. Main dietary sources of folate are liver,
green vegetables, nuts and yeast. Western diets contain ~0.5–0.7mg
folate/d but availability may be lessened as folate is readily destroyed by
cooking, especially in large volumes of water. Folate coenzymes are an
essential part of DNA synthesis, hence the occurrence of megaloblastic
change in deficiency.
chemical formula of Folate (B9)
Diagnosis
Haematological findings are identical to those seen in B12 deficiency—macrocytic, megaloblastic anaemia. Other findings also similar to B12
except parietal cell and intrinsic factor autoantibodies usually –ve.
Reduced folate levels—serum folate levels reflect recent intake, red cell
folate levels give a more reliable indication of folate status.
Causes of folate deficiency
5 intake Poor nutrition, e.g. poverty, old age, ‘skid
row’ alcoholics.
4 requirements/losses Pregnancy, 4 cell turnover, e.g. haemolysis,
exfoliative dermatitis, renal dialysis.
Malabsorption Coeliac disease, tropical sprue, Crohn’s
and other malabsorptive states.
Drugs Phenytoin, barbiturates, valproate, oral
contraceptives, nitrofurantoin may
induce folate malabsorption.
Antifolate drugs Methotrexate, trimethoprim, pentamidine
antagonise folate cf. induce deficiency.
Alcohol Poor nutrition plus a direct depressant
effect on folate levels which can precipitate
clinical folate deficiency.
Management
1. Treatment and support of severe anaemia as for B12 deficiency.2. Folic acid 5 mg/d PO (never on its own—see above), unless patient
known to have normal B12 level.
3. Treatment of underlying cause e.g. in coeliac disease folate levels and
absorption normalize once patient established on gluten-free diet. Long
term supplementation advised in chronic haemolysis e.g. HbSS or HS.
4. Prophylactic folate supplements recommended in pregnancy and other
states of increased demand e.g. prematurity.
all image are come from google image
posted by medica world.com







No comments:
Post a Comment